By Zoisa Fraser
The recent death of a ten-year-old girl at the Georgetown Public Hospital from appendicitis has moved the relatives of an infant who died from the same condition in 2003 to go public, saying that the hospital seemed unable to diagnose the condition properly, especially in children.
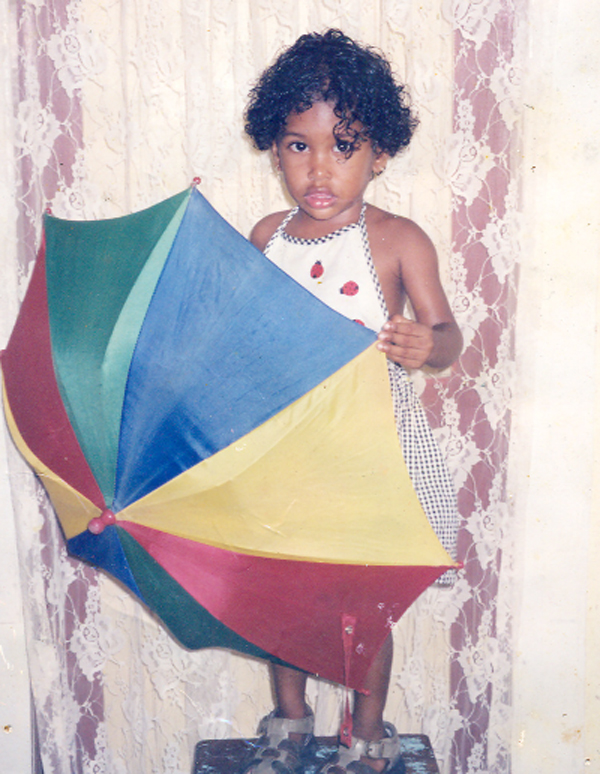
According to the Cummings Lodge family, two-year-old Crystal Stephens died almost one week after she was admitted to the Georgetown Public Hospital in late June 2003, even though she had glaring signs of a ruptured appendix. The family said the doctors were divided on what the child’s condition was, and by the time they decided that it was appendicitis, it was too late. She died on July 3, 2003 before she could have been taken to the operating theatre.
Suzette Stephens, the grandmother of the two-year-old, told Stabroek News that when she read the story headlined “Girl, ten, dies of ruptured appendix” in the June 10 edition of this newspaper, she recalled her own experience at the very hospital almost five years ago. She said the death of her granddaughter was similar to that of ten-year-old Kean Greaves as one doctor had recommended surgery for appendicitis but it was not pursued following the opinion of another doctor. Greaves of Agricola died at the hospital following days of medical evaluation.
For three days, Greaves was taken to the public hospital complaining of an unbearable pain in her tummy and according to her mother, Trudy, doctors looked at her, prescribed tablets and sent her away. On the day they decided to keep her, the child was already far gone and a late rush for surgery was too late. The post-mortem examination revealed that she died from a ruptured appendix and it also showed that her kidney was infected.
Going public
Asked why she came forward now after so many years, Stephens said she and her family have managed to accept Crystal’s death, but she understood what Greaves’ relatives were going through.
She said she wanted the hospital to admit that the doctors were delinquent in both cases and let them face the law so that relatives could get some justice.
“I am very upset over this. We were very shocked when we read it in the paper and after reading the last few paragraphs I burst into tears,” the woman said, adding that she was prepared to support Greaves’ relatives in their quest for justice.
Stephens said that treating appendicitis should not be an issue because an appendix can be removed during a 15-minute surgery.
“It was negligence at that hospital. They should be charged… If they don’t … things like this will continue to happen,” the woman said.
Stephens said she found it difficult to understand how the doctors could not correctly diagnose a ten-year-old child. “This was a big child. This is a clear case of negligence. We are willing to support her [the mother] all the way because this happened to us,” she said.
Stephens opined that the girl’s family should be compensated and the medical personnel who were at fault ought to be fired or placed before the court. Stephens and other relatives had tried getting compensation for Crystal’s death but things did not work out.
High fever
Stephens said that on June 26, 2003, her granddaughter developed a very high fever that was not going away and had also vomited. She said she stayed away from work that day to care for her and took her to the Georgetown Hospital the next morning.
She said that after about three hours, a nurse examined the child and found that she had a 106-degree temperature.
“The nurse pick she up right away and rushed her into the emergency room and instructed me to bathe her with ice (water)… The doctor later said that he suspected appendicitis but he called another doctor and he said no,” the woman recalled. The child was then admitted to the paediatric ward with her temperature still high.
According to Stephens, the second doctor said that she had a respiratory infection and prescribed medication.
“I just knew something was wrong with her and I keep begging them to look at her because she was complaining about her belly,” Stephens said.
Several days later, she said, she pleaded with the head paediatrician to examine the infant again, as her belly was noticeably swollen.
She said an x-ray was done and a series of tests ordered. All this time, her granddaughter’s temperature remained high despite the fact that nurses were bathing her with ice water, two to three times a day.
The woman said that the nurses told her that the child needed blood and plasma because she had problems with her bone marrow. She said that she managed to get 11 pints of blood donated to the institution but Crystal was not accepting the blood and her condition continued to deteriorate.
She died three days later, Stephen said, adding that she had started to look limp, two days before she died.
Informing this newspaper that she was trained in first aid, the woman said the high fever that was not breaking, the vomiting, the swollen belly and pains in that area were all glaring signs that something was wrong with the child’s appendix. The doctors, she said, should have been able to pick this up.
Unacceptable
A report was made to the hospital’s administration but nothing was done, Stephens asserted, until the family approached the Medical Council of Guyana.
Over two years later, on Septem-ber 28, 2005, the child’s relatives received a letter from the council stating that it could not pursue the matter as the hospital’s investigation took a long time and the doctor concerned had left the country. The hospital’s report, which was attached was dated May 10, 2005.
The doctor referred to had resigned from the hospital on September 24, 2003, a little over two months after the infant had died.
According to the report, which was addressed to Dr MY Bacchus of the Medical Council and signed by Dr Rambaran, Crystal was diagnosed with a lower respiratory infection and emetic syndrome after being examined in the emergency room and was admitted on June 28, 2003.
“Paediatric medicine entertained the possibility of a surgical abdomen and referred the child for a surgical opinion on July 1, 2003,” the report said. (This was two days before she died).
Medical Officer General Surgery, Dr R Ramraj, evaluated the child on July 1, and diagnosed appendix mass and recommended non-operative treatment including antimicrobials, the report said, adding that that doctor did not inform his consultant, P Santosh about the referral. “Dr R Ramraj erred in not discussing this patient with his consultant.”
The report said paediatricians were investigating a hematogical disorder because of the low white blood cell count of 1,200.
“In light of the post-mortem findings of bacterial peritonitis secondary to acute appendicitis it is apparent that this child was admitted with severe sepsis. In severe sepsis abdominal signs are not apparent and this together with the low white cell count led to delay in the diagnosis. It was concluded that Dr. R Ramraj would be censured for failure to discuss this referral with his consultant…” the report said. The report did not indicate whether in fact the doctor was censured, but added that he resigned on Septem-ber 24 that year.
Following Greaves’s death last week, Dr Rambaran was contacted and he said an investigation would be launched.