Dear Editor,
Since 2015, the framers of the National Mental Health Action Plan (NMHAP) 2015-20 have been talking about shifting towards a community- based mental health care model instead of institutionalised care. The two-year old coalition administration must be applauded for its quick action in addressing the mental health crisis which is crippling our nation. However, more education is needed for the populace and even more for service providers so they can recognise when people are in crisis. There is a need for objective and subjective data collection in order to make a proper diagnosis.
After perusing the NMHAP document, I was enthralled with this elaborate, ambitious, and comprehensive instrument which has been in the pipeline since 2008. Given the timeline it took to prepare such a user friendly instrument, looking ahead to 2020 we should anticipate at a minimum of a clean-up of the most severely affected among the mentally ill—our growing street population.
There were a few high point in the NMHAP that particularly grabbed my attention:
- There are no independent review bodies to protect the human rights of users of mental health services.
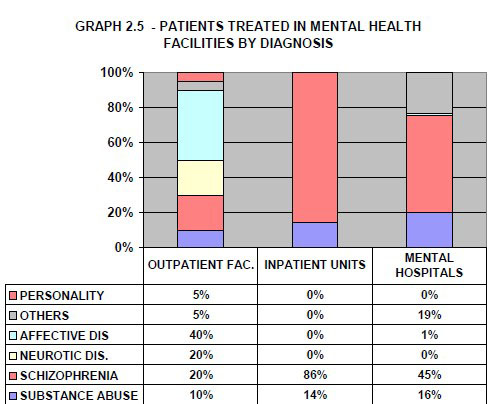
- The patients admitted to mental hospitals belong primarily to the following two diagnostic groups: schizophrenia and delusional disorders (45%) while the others include epilepsy, organic mental disorders and mental retardation (19%).
- The most frequent admission diagnosis is psychosis (86%) followed by substance-related disorder (14%).
- Although at least one medication from each class of psychotropic drugs is available at all mental health facilities as well as most primary and secondary care facilities in Guyana, there are no guidelines or protocols for the use of psychotropic drugs, and few health or specialized mental health workers have received any training in the rational use of these medications.
- In terms of available treatments, both outpatient facilities offer limited psychosocial treatments and both have access to at least one psychotropic medicine of each therapeutic class (anti-psychotic, antidepressant, mood stabilizer, anxiolytic, and antiepileptic medicines) year round. The GPHC has consistent access to all psychotropic medications listed in the National Formulary, which includes at least one psychotropic medicine of each therapeutic class.
- Mental health in primary health care, both physician-based primary health care (PHC) and non-physician based PHC clinics are present in the country. Neither have assessment and treatment protocols for key mental health conditions.
According to the WHO-AIMS report, Guyana’s mental health network consists of 1 mental hospital (with 240 beds), 2 outpatient facilities, and 1 community-based psychiatric inpatient unit (with 4 beds). Four times more outpatient care is provided in the country (with 274.9 outpatient users per 100,000 population) than inpatient care (59.2 and 33.7 users per 100,000 in the community- based inpatient unit and mental hospital, respectively).
Summary for Graph 2.5:
The distribution of diagnoses varies across facilities: in outpatients facilities affective disorders are more prevalent, the majority of patients admitted to the community inpatient unit have a diagnosis of psychosis, and in mental hospitals schizophrenia and “other” diagnoses are most frequent.
Source: Assessment Instrument for Mental Health Systems WHO-AIMS). Georgetown, Guyana, 2008
There is no doubt with a shortage of trained professionals in this field, the task of simply diagnosing is a mountainous challenge to achieve by 2020.
Mental health is a vast field and often treatment boils down to judgment by the treating staff ‒ here treating staff refers to the professional trained in the area of mental health. The following pointers are to sensitise the general public on a few important markers:
- The need for protocols and guidelines is crucial so that treating staff know and understand what they’re supposed to do and not deviate from it.
- Protocols and guidelines hold people accountable.
- The danger is when personal opinion kicks in, treating staff will begin to do their own thing.
- Whenever treating staff are in doubt they will have something to fall back on.
- Treating staff need to recognise when a patient is decompensating; they should not have to be operating in crisis mode.
- Standing orders (a written document containing rules, policies, procedures, regulations, and orders for the conduct of patient care in various stipulated clinical situations) must be fully enforced at all times when dealing with the mentally challenged population.
- In order to arrive at a diagnosis a thorough assessment must be done first; if a patient doesn’t have a diagnosis how do you treat them?
- Treatment falls into three categories: (a) talking therapy, (b) medication management, and (3) a combination of both treatment types.
All psychotropic drugs have side effects, and can often produce psychosis. At times, one drug may contradict another. Blood levels should be checked to ensure therapeutic levels of the drug in the blood are achieved, especially when patients are prone to seizures. Work must be done before administering any psychotropic drug. When patients are admitted to any mental health institution and presenting in a psychotic state, the protocol is to observe the patient for 24 hours in the event they may have skipped their meds or are on street drugs. Introduction to psychotropic drugs at this early stage is detrimental to the patient.
I sincerely hope that this information is beneficial to the consumers and service providers of mental health services.
I met Adam (21) the other day; he experienced a meltdown in 2016 and passed through the outpatient psychiatric clinic. Three weeks ago he relapsed and has not been able to walk or complete hygienic functions such as brushing his teeth without assistance. Without appropriate protocols and guidelines in place, we can be creating illness.
Yours faithfully,
Ingrid Goodman
Executive Director
Patois/Women’s Refuge