A performance audit into the management of drugs and medical supplies at the Ministry of Public Health and Regional Health Facilities for the years 2015 to 2018 found that millions of dollars were wasted from spoilt or damaged supplies owing to poor storage.
The performance audit report was compiled by the Auditor General and laid in the National Assembly yesterday.
The report said that the Ministry of Public Health and the Regional Democratic Councils are responsible for buying and distributing drugs and medical supplies to citizens. It noted that over $3 billion was spent from 2015 to 2017 to buy supplies and a performance audit for the period 2015 to August 2018 was done to assess how well the supplies were managed.
Auditor General Deodat Sharma, in the report, said “millions were wasted from spoilt and damaged supplies due to poor storage, which left Guyanese without needed supplies. Essential items were out of stock for long periods, and suppliers did not deliver items valued in the hundreds of millions of dollars. The audit work was hampered repeatedly because the Ministry and the Councils did not provide requested documents and did not respond to the audit reports.”
The review period is from January 1, 2015 to August 15, 2018. During the period under review, there were three Ministers of Public Health, Dr George Norton, Volda Lawrence and Dr Karen Cummings, serving under the APNU+AFC government.
From January to May 2015, Dr Bheri Ramsaran served as Minister of Health under the PPP/C administration.
The performance audit, according to the report, was also done to determine whether the Ministry of Public Health and the Regional Democratic Councils procured drugs and medical supplies in an economic manner and managed the receipt, storage and distribution efficiently and in compliance with policies, international best practices, relevant laws, regulations and guidelines.
The Auditor General said that audit checks were done in October 2020 as part of the review process.
The Ministry of Health’s Materials Management Unit is responsible for the distribution of drugs and medical supplies to 356 health facilities across the ten Administrative Regions of Guyana. During the course of the audit, 50 of those facilities were visited.
For the years 2015 to 2017, the Ministry and the Regional Democratic Councils were allocated sums totalling $11.604 billion for the procurement of drugs and medical supplies. During the review period, the ministry entered into 318 contracts valued at $12.132 billion over the three years under review, with both national and international suppliers. The report noted that the contracts did not include provisions to prevent delays by contractors nor measures to recover any overpayments. Specifically, the contracts had no start and end dates or penalty clauses.
However, included was a clause stating that delivery will be made at the request of the Ministry. The failure to include specified dates and penalty clauses in contracts denied the Ministry recourse in dealing with delinquent suppliers, the Auditor General opined.
As a result, it was recommended that contracts should include contractual terms and conditions that will protect the Ministry from delinquent suppliers.
Market prices
The report found that the ministry paid higher than market prices owing to its restricted tendering method. In 2017, the Ministry wrote to the National Procurement and Tender Administration Board requesting approval for the suppliers to be invited to bid for 13 “emergency” pharmaceutical supplies.
Approval was granted in May 2017, and bidding documents were sold to International Pharmaceutical Agency, Caribbean Medical Supplies, ANSA McAl Trading Ltd, Global Healthcare Supplies Inc, Meditron Inc, and HDM Labs Inc to bid.
International Pharmaceutical Agency, Caribbean Medical Supplies, and ANSA McAl Trad-ing Ltd were the only respondents and the contract was not awarded owing to the companies not meeting the evaluation criteria. Approval was granted for retendering and HDM Labs Inc was the only respondent. The contract was awarded to HDM Labs Inc and the Auditor General found that a significantly higher price was paid by the Ministry.
The Auditor General said that the Procurement Act 2003 was breached when the Ministry engaged three suppliers to deliver items valued at $41.180M before the tender board awarded six contracts valued at $104.140 million.
“The Ministry awarded two contracts more than thirty days after the supplier commenced delivery of the drugs. We could not determine whether the Ministry received the best price for each item since there was no evidence that prices were evaluated before deliveries to determine the most competitive price among suppliers,” the report stated.
Additionally, the ministry did not provide the files for thirty contracts totalling $22.163 million to the auditors. Auditors requested over 1,800 payment vouchers for the years under review from the various Regional Democratic Councils but only received less than 400 totalling $124 million.
Auditors found that the inventory management systems were poor and that there was no evidence that the Ministry and the Regional Democratic Councils coordinated procurement activities and maintained a comprehensive database of procurement activities.
Files
The Auditor General concluded that the ministry’s failure to present Ministerial Tender Board files and evaluation reports for contracts awarded affected its review of the procurement process.
“We could not determine whether invitations to tender were widely circulated in newspapers because we did not receive the invitations. In addition, the Ministry was not protected from defaulting suppliers because contracts awarded were deficient in performance criteria, such as start and end dates and penalty clauses.
“The Ministry did not always get the best prices for purchased items, as prices paid for emergency pharmaceuticals were much higher than those quoted by other suppliers. Further, there were instances where suppliers delivered the items to the Ministry days before the award of contracts. As a result, we concluded that the Ministry and the Regional Democratic Councils did not efficiently procure drugs and medical supplies and properly account for the items purchased,” the report stated.
Poor management
The report said that the suppliers did not always fulfil their contractual obligations and could not be penalized.
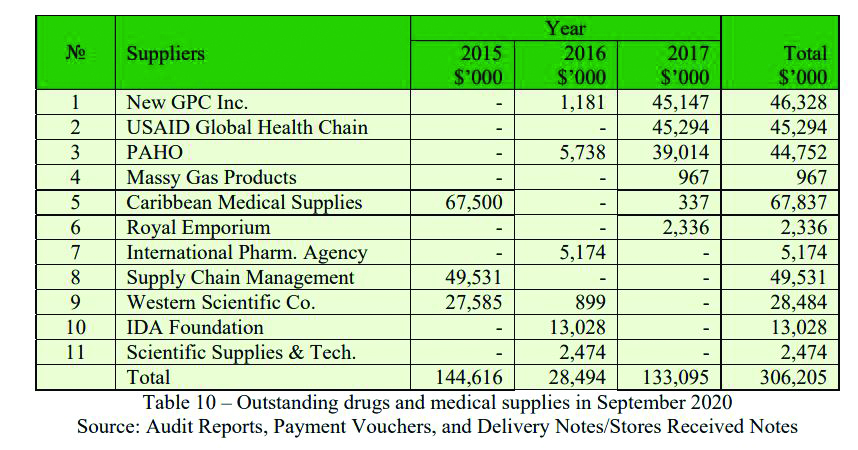
At the end of August 2018, 12 did not deliver drugs and medical supplies valued at $346 million from purchases made from 2015 to 2017. According to the report, one supplier delivered $40 million of supplies in October 2020 leaving outstanding supplies valued at over $306 million still to be delivered. The outstanding drugs and medical supplies account for 47% of the amount procured during that period.
Insert table saved as table1
The report revealed that a $409.4 million contract was awarded in August 2017 to procure drugs and medical supplies with a delivery deadline date of no later than 22 September 2017. The first set of deliveries was done in October of the same year. The supplier fulfilled the obligations under the contract in March 2018, six months after the delivery date. The Ministry still owes the supplier $66.2 million.
From 2015 to 2017, the report said, the Regions got $5.158 billion to buy drugs and medical supplies and entrusted $4.517 billion to the Ministry. The balance of $641M was available to be used whenever items were out of stock at the Materials Management Unit. The Unit was required to meet the demands of the Regional Health Facilities.
The auditors found that the Materials Management Unit oftentimes was unable to meet the demands of the health facilities. As a consequence, the health facilities were not able to meet the needs of citizens.
“We found that essential drugs were out of stock for long periods, ranging from two months to five years. We noted that the Linden Hospital Complex was out of anti-snake venom injection for almost five years. At the Bartica Hospital, Quinine Sulphate to treat malaria was out of stock for three years. For two years, the Suddie Hospital did not have in stock potassium chloride injections to treat low blood levels,” the Auditor General informed.
Poor storage
The auditors found that poor storage practices over the years resulted in the Ministry suffering losses from expired drugs and medical supplies. Auditors examined the Expired Medicines Valuation Report to assess the effects of expired drugs and medical supplies on the health sector.
In three years, there were 886 expired drugs and medical supplies with only 488 items with a value of $690m reflected on the report. The value of almost 400 items was unknown since the Materials Management Unit failed to provide the cost to them. It was discovered that the cost of each drug and medical supply was not inputted in the Management Accounting Computerized Software at MMU for 2015 and 2016 and as such auditors failed to validate the accuracy of $950 million in expired drugs and medical supplies from 2015 to 2017.
“Except for Cotton Tree and Britannia Health Centres, the other health facilities had large quantities of expired drugs on hand. The value of the drugs was unknown because none of the facilities presented a costed list to us. Further, there was a lack of accountability on the part of health facilities to keep records of expired drugs and medical supplies. We found no system in place to promptly remove damaged and expired drugs and medical supplies at health facilities. At the West Demerara Regional Hospital, we noted items were on hand even though they had expired since 2010,” the report highlighted.
Auditors also found that the ministry failed to properly assess its rented bonds and drugs were stored in termite-infested facilities. Additionally, no systems were in place to properly sort and dispose of the expired drugs and medical supplies.