With reports of negligence in hospital wards, callous treatment of patients and a string of recent maternal deaths in the country the image of the nursing profession has been bruised. President of the Guyana Nurses Association (GNA) Joan Stewart says they will work on repairing it, but the problems are chronic.
The majority of nurses in the system have less than ten years experience and migration continues to cripple the profession. Health Minister Dr Leslie Ramsammy is on record as saying that about $600M is spent on nurses’ education annually and about half of that is lost in migration for the same period.
“We are concerned about the maternal deaths… women are not supposed to be dying,” Stewart said, noting that there was a lack of experience in the profession. Training was not an issue in Guyana, Stewart asserted, noting that the health sector continued to churn out nurses in large batches every year. She believed the real issue was the quality of the training and the conditions under which nurses were being trained.

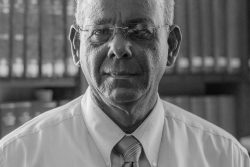
Stewart, an experienced nurse and skilled midwife, has been in the system for many years and she told Stabroek News during a recent interview that questions had been raised about the tutor to student ratio, which was estimated to be as high as one tutor to 150 student nurses. She recalled that in the past the ratio was one tutor to around 25 student nurses.
The GNA President observed that some people were just working in the profession because they considered it a ticket out of the country. The criteria by which nurses were selected was not “what it used to be,” she said, adding that many years ago people had to demonstrate certain qualities before they were allowed to train as nurses.
Stewart said her association considered itself an important stakeholder in helping Guyana to achieve the targets set for maternal healthcare in the Millennium Development Goals (MDGs). She said that the attitude of some nurses was something the profession continued to grapple with, and she frankly stated that some people “are not cut out for nursing.”
She said too that those fresh out of training, many of whom were currently working the wards, needed constant reminders of nursing ethics. Staffing was also a problem and the ratio of patients to nurses at the public hospital maternity ward was high; midwives, she pointed out, had to do manual monitoring.
But there were “other issues” in the profession which needed to be addressed, Stewart said, pointing to remuneration packages and the general treatment of nurses. She said some of the nurses felt that they were underpaid and unappreciated, which was often cited as among the key reasons why they migrated, and/or why some were on the job “with attitudes.” She said government needed to implement programmes to retain nurses and suggested low-term loans for housing as a good initiative. “They need to invest in nursing because it is an important [part of] the health sector,” she added.
Following the rules
Stewart said she had not been privy to any of the findings of internal reports which were conducted following the recent maternal deaths and therefore, “cannot say what went wrong.” However, she ventured that some nurses appeared not to be following the rules.
“We work in accordance with rules and if people stick to them we should not have the problems we are having…” she observed. She said the Health Ministry had been doing quite a lot work to minimize the incidence of maternal deaths over the years, noting there were many pillars on which the maternal healthcare programme rested.
The safe motherhood programme which addressed family planning was an important pillar which encouraged women to plan their pregnancies. She said that if a couple decided to have a baby both parents should ideally be screened to determine their medical history. She explained that the woman should know her HB (haemoglobin levels); her HIV status; her blood type; and whether she was diabetic or hypertensive, among other things.
But this information was usually only obtained when the pregnant woman turned up at the clinic for pre-natal care. She said the doctors would seek additional information during that time which included whether the woman had a previous cesarean birth and/or any abortions. Accord-ing to her, some women continued to show up late at the clinics.
Stewart said problems were being reported during the period when women went to deliver their babies, noting that the woman had to be monitored routinely during this period, particularly when she was in active labour. She said that a nurse should check the baby’s heartbeat and the mother’s blood pressure every half hour, in addition to monitoring contractions and conducting regular vaginal examinations.
There are ‘red flags’ when nurses needed to make critical decisions and call in doctors. She pointed to the foetal heart rate going down; a woman’s pressure going up; a woman not dilating and or if she was exhausted. She said there were other signs which indicated that both mother and child were in distress. “Nurses would follow the signs and make an intervention because when they intervene would determine how things turn out,” she explained.
Stewart made the point that nurses were not always the culpable party when something went wrong during delivery but that “we are usually criticized.” She said some nurses suffered when women died on their hands, and they were left traumatized for some time without any counselling. She referred to the incident involving fellow nurse Amsterdam, saying that people had already started asking if the nurses could not save one their own, “who can we save?”
Creating changes
Stewart called for the inclusion of a GNA member on the committee that review-ed maternal deaths saying they too would like to be made aware of what goes wrong in the system. Alter-natively, she said the findings of the reports could be sent to them. According to her, GNA would be able to hold discussions with the midwives arm of the body and analyse each case in an effort to bring about changes.
She also spoke of the ALARM programme which the Health Ministry had initiated (Advances in Labour and Risk Management) which coordinates the monitoring process for deliveries, but Stewart said she had no idea how many nurses were tapping into what was learnt during those sessions.
Currently GNA was looking at the midwifery curriculum to determine whether changes should be made and she disclosed that they were considering training for midwives in CS (C-Sections) as well as manual removals of the placenta. She said some midwives were afraid to commence the training, but others would like to learn.
GNA was also considering a mentoring programme for members of its youth arm where experienced nurses would offer guidance whenever it was needed; “We would just be a call away…” she said. Further, the association was looking at a leadership programme to help young nurses to be more innovative and make better decisions.
But according to Stewart, “It all comes down to patient care.” She said that every patient lying on a hospital bed was “someone else’s loved one,” adding that nurses are told to treat patients as if they were family.