A performance audit into the management of healthcare waste at hospitals conducted from January 2017 to July 2019 found that the overall system was poor and placed healthcare workers and patients in harm’s way.
Auditor General Deodat Sharma, in his report on the audit, said that all stages in the management of healthcare waste were lax, creating human and environmental health hazards. He noted that policies and plans were not established to efficiently and effectively manage waste activities, resulting in a lack of coordination among officials.
“The absence of waste collection schedules and monitoring at each hospital led to ad hoc collection patterns which put at risk the health of patients and workers. Poor segregation systems resulted in injuries to workers from [sharp objects] in bags. The audit work was repeatedly delayed because hospitals did not provide requested documents and did not always respond to the audit findings,” the Auditor General said.

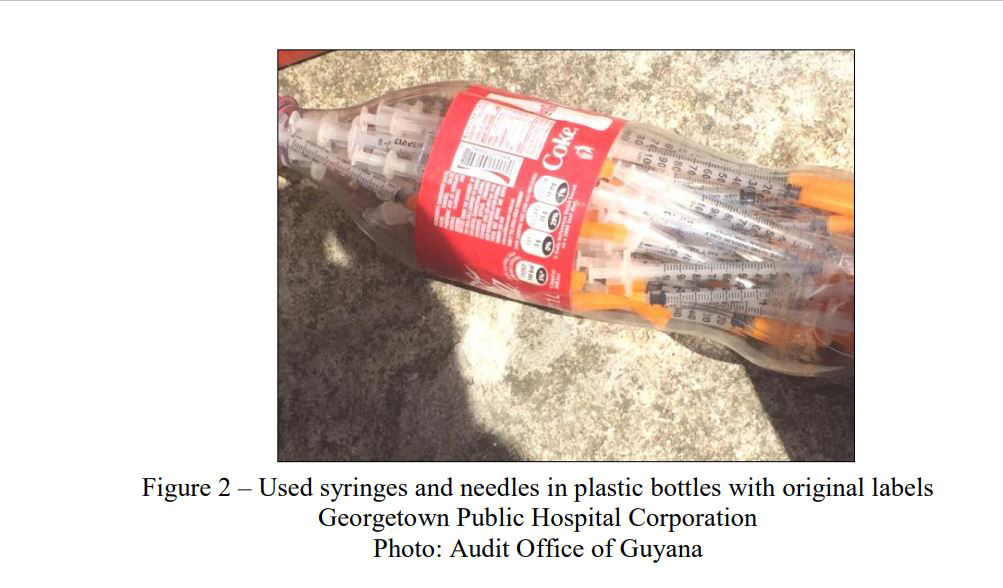
According to the report, inadequate storage space and poor storage practices were to be blamed for large amounts of sharps containers being littered in the hospitals. It was noted that the containers with untreated infectious waste were stock-piled for months in rooms and hospital compounds. Additionally, used syringes and needles were in plastic soda bottles used as sharps containers, particularly when hospitals were out of stock of the required containers.
The country’s largest medical institution, the Georgetown Public Hospital Corporation (GPHC) was flagged for the use of Coca-Cola bottles with original labels to collect sharps waste. The Auditor General said that the bottles were not labelled and sealed to prevent persons from removing the used syringes and needles and as a result, used syringes and needles were easily accessible to persons, which could have resulted in theft and infections if used.
“Prolonged stock-outs caused by shortages or short supplies led to personal protective equipment being unavailable to waste handlers. Waste handlers wore part and sometimes none of the personal protective equipment when executing their duties. Management’s failure to monitor waste handling activities resulted in waste handlers’ exposure to infections.
“Waste was dumped on the floor after treatment. We found that this unsatisfactory situation at the Georgetown Public Hospital Corporation was because the shredder and belt of the autoclave were out of order. The machine was not working at capacity, which caused containers of untreated waste to accumulate, resulting in health and environmental risks to waste handlers,” the report highlighted.
The audit focused on the administration, segregation, transporting, storage, and disposal of healthcare waste at five hospitals – West Demerara Regional Hospital, Georgetown Public Hospital Corporation, Diamond Diagnostic Centre, New Amsterdam Regional Hospital and Linden Hospital Complex.
At the time of the Audit, the APNU+AFC was in power and the then Ministries of Public Health and Communities were responsible for the regulation and oversight of waste management. The Auditor General said that a national waste management plan was not presented to auditors despite all healthcare centres being mandated to have one.
Section 4 (e) of the Ministry of Health Act of 2005 requires the Ministry “to develop and ensure the implementation of the National Health Plan and other action plans and directives, including human and all other resource required necessary for assessing, monitoring and implementing such policies and plans, founded on population-based needs for health care programmes, services and facilities.”
The report related that the Linden Hospital Complex presented a draft waste management plan but there was no evidence to indicate whether it was approved for implementation. New Amsterdam, West Demerara, and Diamond Hospitals did not develop waste management plans for the period under review. The Georgetown Public Hospital Corporation presented a single-page document purported to be the hospital’s waste management plan and an examination of the
document revealed that it was the findings from an inspection conducted to evaluate the hospital’s practices and compliance with national guidelines.
The Diamond Diagnostic Centre failed to present auditors with a waste management plan.
In response to the Auditor General’s findings, the Linden Hospital adjusted its draft plan and approved its implementation while the Diamond Diagnostic Centre developed its plan in 2018. The GPHC presented an unapproved plan.
In addition to the lack of waste management plans, the Auditor General also found that some of the hospitals lacked a proper waste management committee. The institutions were also flagged for failure to present their standard operating procedures (SOPs) to the audit office. Additionally, the institutions were flagged for not properly documenting medical waste.
“The Ministry of Public Health and the Ministry of Communities did not efficiently regulate health care waste at hospitals. A policy was not in place to manage waste. Further, a national medical waste management plan, and individual management plans from hospitals for good waste management practices, were also not provided for audit. In addition, there were stock-outs of personal protective equipment at four of the five hospitals,” the report concluded.
The audit team visited the hospitals for three months to determine waste collection patterns and observed that GPHC, WDRH, LHC and New Amsterdam Hospital collected general and hazardous waste containers twice daily. The waste was placed in larger containers at a central storage site before being removed at varying times during the day. However, labels were not on the containers to show the type of waste.
At the Diamond Diagnostic Centre, it was observed that there was no waste collection schedule. In fact, the hospital officials said that once filled, only then are containers and bins removed from wards, departments, and clinics. Thus, containers with waste were in the areas for longer than a day. This practice put at risk the health and safety of staff, patients, and visitors to the hospital, the report noted.
Appropriate containers were also not used to store the medical waste.
The Diamond Diagnostic Centre, had no designated container or trolley fitted with wheels to transport waste. Waste was carried by hand or in the wheelchair used by patients.
“The West Demerara, New Amsterdam, and Linden hospitals used incinerators for burning waste. The hospitals did not have environmental authorizations or permits from the Environmental Protection Agency to operate the incinerators. The use of incinerators released harmful chemicals and pollutants into the air, water, and even the food supply. Consequently, the chemicals and pollutants could have gotten into citizens’ bodies when they breathed, drank, and ate contaminants. As a result, we conclude that the unauthorized use of equipment by hospitals to treat waste posed environmental and health risks to persons,” the report highlighted.