With one of the highest suicide rates per capita in the world, Guyana has been making very poor steps in addressing mental health issues and the state of its treatment hospital has been described as “sad”.
The country’s Chief Psychiatrist, Dr Bhairo Harry yesterday called out the authorities for inconsistent action on addressing the plethora of mental health-related illnesses.
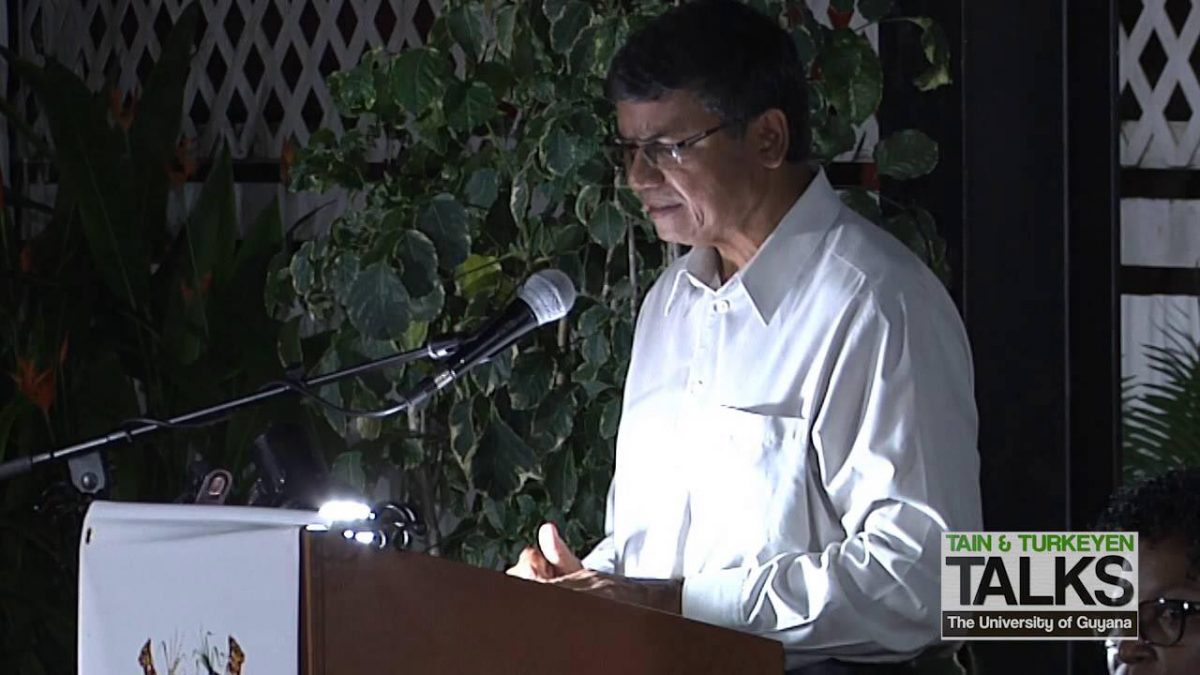
Dr Harry told the opening of the Guyana Mental Health and Well-being conference that several plans had been put in place to further develop the level of psychiatric care in Guyana but most, if not all, of those plans have been abandoned.
“Now many things we have started and for different and unknown reasons these things are being left down,” Dr Harry told the gathering at the Arthur Chung Conference Centre, Liliendaal, East Coast Demerara.
Pointing to one of the many programmes that were abandoned, he explained that the National Psychiatric Hospital (NPH) at New Amsterdam in the East Berbice region was supposed to be modernised to function as a National Psychosocial Rehabilitation Centre.
“The idea was to study each case and classify all these and then create a neuropsychiatric service, psychogeriatric service, substance use/abuse service and then the acute care service and that alone could have reduced 200 psychiatric beds to probably 60 or 80. Then with that kind of approach or thinking was that the people would have gotten better care. A few years ago, (it) fell apart,” he related.
For many years, Dr Harry served as Guyana’s lone psychiatrist. Now there are 14 psychiatrists spread across the country to serve its 786,000+ citizens.
Currently, mental health care is being delivered through outreaches in various regions. With 14 psychiatrists, including two child psychiatrists, clinics are being held in Regions One (Barima-Waini), Five (Mahaica-Berbice), Seven (Cuyuni-Mazaruni), and Nine (Upper Takutu-Upper Essequibo).
There are resident psychiatrists in Region Three (Essequibo Islands-West Demerara) which has two sites and a third under construction, at the NPH in Region Six (East Berbice-Coren-tyne), Region Four (Demerara-Mahaica) at the Georgetown Public Hospital Corporation (GPHC), and in Region Ten (Upper Demerara-Upper Berbice)
However, no psychiatric services are being offered in Region Eight (Potaro-Siparuni).
The NPH was created as a result of the Mental Health Ordinance of 1930 and is still the only facility solely dedicated to catering for persons with mental health issues. The archaic Mental Health ordinance, which has been revised several times but never made it to the legislature for amendments, grants a Magistrate the power to order that someone be made a patient at the NPH after examination from medical practitioners.
“…the Magistrate shall have the same powers as if the person alleged to be of unsound mind were a person against who a complaint had been made for an offence punishable upon summary conviction…any person who has been adjudged a person of unsound mind under this section shall be delivered into the custody of the police or other authorized person together with the warrant and the medical certificates or certificate of his unsoundness of mind and they shall be responsible for his safe conduct to the Mental Hospital…” the Mental Health Ordinance states.
In relation to the NPH, Dr Harry lamented that the institution is currently in a “sad state”.
“The National Psychiatric Hospital, it’s a sad place, very sad place. Work has been done many times (there and) physical structures have been erected but then did we accompany that by improving the number or quality of staff? The answer is no. So, we basically have an institution where basically 70% of the people are not needing to be there but they are there,” he lamented.
The state of the NPH has been under scrutiny for years. In June of this year, 41-year-old Ryan Sunthgolam of Canefield, East Canje was killed and Steve Lionel Roberts, 38, was injured. The men were attacked when a patient pulled out a window and grill mesh and inflicted injuries on them. Shortly after, 11 patients were hospitalised after a fire broke out at the institution. Four of the residents there suffered burns about their bodies.
Serious questions have been raised about the staffers’ ability to deliver care at the institution and protect its residents, some of whom are violent, from harm.
“We need a functional plan for the national psychiatric hospital and our mental health plan is not perfect, we need to update that and I think PAHO is helping us with that now,” Dr Harry said.
Changes
Guyana’s laws criminalise attempted suicide and for years, politicians, from both sides of the aisle, have called for decriminalisation. However, no steps were taken to have that done.
Dr Harry used the platform to also advocate for the enactment of legislation which places mental health and its related illnesses on the front burner. He said that the national suicide prevention plan needs a lot of work to address the realities of the situation in Guyana.
“We are assisted by the Dalhousie University (in Cana-da) and started doing work. They developed a national mental health strategy, national suicide prevention plan, they reviewed our archaic Mental Health Ordinance of 8 March 1930. Since then we have been reviewing it and it went through many stages. It went through three Ministers’ (of Health) hands.
It is only now getting some action and hopefully, this will be real action. We recognize all these shortcomings with the old archaic ordinance, one of them being the criminalization of suicide attempts. Our new mental health bill will be more (patient-friendly),” the psychiatrist related.
He added that they are hoping to have the new Suicide Preven-tion Bill tabled in the National Assembly by the end of 2021.
Dr Harry reiterated that greater emphasis should be placed on addressing mental health issues because it is something that almost every person battles.
In August, Attorney General Anil Nandlall announced that the Mental Health Act will be revamped, with specific attention being paid to persons in the penal system. He had said that the Mental Health Act is completely out of sync with the realities on the ground.
Yesterday, Dr Harry seemingly agreed with Guyana’s laws being completely out of sync adding that even the available research data does not reflect the realities on the ground. He said that there is very little research data on mental health in Guyana and identified the need for such.
However, Dr Harry did indicate that there are small research studies being undertaken by medical students and residents. He added that between 2003 and 2012, he conducted three studies in an effort to influence policy but those studies also had their limitations.
“Research very much needed. We have not done very much research. We didn’t have the time, now we have the personnel but not the time… There is so much to be done. We have very limited amount of policies when it comes to mental health, especially the usage of psychotropic drugs,” he said.
The psychiatrist also lamented the fact that Guyana does not have the facilities to offer psychiatric care to prisoners despite now having a forensic psychiatrist. He explained that there are just two beds in the prison to house prisoners with mental health-related issues.
In relation to the issue of prisoners being mentally ready to be allowed back into the general population following their release, it is unclear whether they are evaluated and even if they are, then the steps to treatment are vague.
In May, Ronald Wong and his uncle Leonard Reece were discovered dead in their home at Coomacka, in the Demerara River. Wong had recently been released from prison for attempted murder and went to live with his uncle. Wong, who was said to have been of unsound mind and had special needs, was previously incarcerated after being convicted of attempted murder. It is believed that Wong was responsible for the death of his uncle.
Sabotaged
Dr Harry related that the plan for the next five years was to have a psychiatrist in every Regional Hospital in Guyana and in 10 years, a psychiatrist in every district hospital. However, he said that the plan was sabotaged.
“For a couple of years, I was sabotaged because doctors were not released into my programme. Once they came to the post-grad programme they were not being released. If they were, we would have had a better prognosis. We are now stronger and we are doing better and there is no turning back,” he said.
The post-grad programme he referenced is one he developed with the McMaster University in Ontario, Canada. Thus far, four persons have graduated from the programme and there are currently 5 in the first year and 1 in the second year.
“We have been working and things have been happening and then at a certain point in time, sometime around 2014, like the gearbox got some problem and things stopped happening. By 2015 I don’t know if they change from automatic to stick gear or what it was but things paused and we lost a lot of time. We are now trying to get back on track,” Harry said.
He added that the doctors are now better equipped to handle mental health issues since there is increased training in the field. However, he did acknowledge that the mhGAP Intervention Guide seems to be providing very little success.
mhGAP Intervention Guide outlines signs that general medical practitioners should identify before referring someone to seek mental health care. (Lakhram Bhagirat)